48 year old male with abdominal distension since 20 days
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Case presentation -
A 48 year old male resident of Chityala , auto driver by occupation came to OPD
Chief complaints -
- Abdominal distension since 20 days
- shortness of breath since 20 days
- decrease frequency of micturition since 20 days
- decrease urine output since 3 days
- blood in stools since 3 days
History of presenting illness :
Patient was apparently asymptomatic 20 days back , then he developed abdominal distension , which was insidious in onset , progressive to present size , associated with loss of appetite
Then he developed SOB 20 days ago , insidious on onset , initially of grade 2 which progressed to grade 3 relived on rest
Patient complains of decrease in urinary frequency (1-2 episodes / day ) since 20 days , decrease in output since 3 days. Bright red blood discharge ( few drops ) after passing stools . Solid consistency. Not bile stained
B/L pedal edema extended upto knee , pitting type , relived after walking. No aggravating factors
No H/o abdominal pain , fever , constipation , weight loss , nausea , vomiting , dysphasia
No h/o chest pain , cough , orthopnea , PND , platypnea, palpitations, light headedness , giddiness
No h/o pain during defecation , burning micturition
Past history :
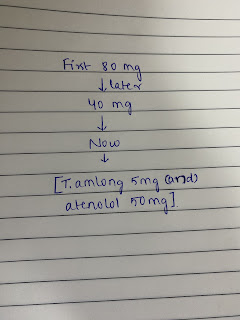
K/C/O of hypertension
Diagnosed 10 years ago
Rx : telma ( amlodipine + atenolol )
VITALS
TEMP - a febrile
HEART RATE -72bpm
PULSE PRSSURE -130/90mmhg
RESP RATE -16cpm
Systemic examination :
Per abdomen
Inspection -
Shape : distended uniformly
Dilated veins are seen
Spider navi is present
Umbilicus - flattened
Abdominal movements are equal
No scars , swellings , visible pulsations
No stretch marks are seen
Palpation -
No local rise of temperature
No tenderness
No rebound tenderness
No palpable swellings
Liver , spleen - not palpable
Percussion -
Shifting dullness - present
Fluid thrill - present
Auscultation-
Bowel sounds - heard
Cardiovascular system -
Inspection -
carotid pulse is seen
JVP visible on sitting
B/L chest movements are equal
Palpations -
Apical impulse felt : 5th Intercoastal space ; mid clavicular
Auscultation -
S1 , S2 heard
No murmurs heard
CNS EXAMINATION









Comments
Post a Comment