55 yrs old male with CKD and SOB
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE PRESENTATION
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan .
55 yrs male patients came to opd with
Chief complaints :
-back pain since 3 months
-reduced sleep since 3 months
-sob since 1 month
- b/l pedal edema since 1 month
History of presenting illness :
Patient was apparently asymptomatic 3 months back then he developed back pain which is insidious in onset , which started with lower back pain then after 1 week radiated upwards, aggravated on prolong sitting and during physical activity , relieved on rest and supine position. He had reduced sleep due to back pain
Then later he developed sob which is insidious in onset , gradually progressive from grade-1 to grade -3 , aggravating on physical activity , no reliving factors
Later he developed b/l pedal edema is developed 1 month ago which is pitting type extended Upto knee
No h/o cough , fever , vomitings , nausea , palpitations , burning micturition
Past history :
He is a known case of hypertension and diabetes
No h/o asthma , epilepsy , tuberculosis
Family history :
No significant family history
Personal history :
Diet - mixed
Regular bowel and bladder movements
Reduced sleep
Addictions - occasionally drinks alcohol
Normal appetite
No allergies
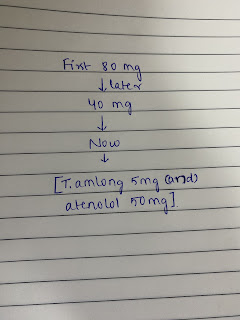
Treatment h/o -
Clonidine - 0.1 mg
Undergoing heamodialysis
General examination :
Patient is conscious , coherent , cooperative
Moderately built and moderately nourished
Pallor present
No icterus , no cyanosis , no clubbing , no lymphadenopathy
Vitals
Bp: 110/70 mmhg
Temperature - afebrile
Rr- 16 cpm
Hr - 80 bpm
Systemic examination -
Respiratory examination:
Inspection -
Upper respiratory tract :
Normal
Lower respiratory tract :
Chest appears to Be symmetrical
B/l chest movements are equal
Chest shape appears to Be elliptical
Trachea appears to Be normal
Apical impulse is seen
No h/o drooping of shoulder , no spine deformities ,
no visible scars , sinuses , dilated veins , nodules , swelling
No hallowing is seen
Palpation -
Confirmed inspiratory findings
Trachea - midline
B/l chest movements are equal
No local rise of temperature
No tenderness , no crowding of ribs ,
Vocal fermitus - normal
Percussion -
Resonant
Auscultation -
B/l vesicular breath sounds
Vocal resonance - normal
Per abdomen -
Non tender , soft
Cardiovascular system -
S1 , s2 heard ; no murmurs
Central nervous system -
No focal deficits
Provisional diagnosis -
CKD with sob


Comments
Post a Comment